Caregiver Burden to Burnout
According to the American Psychological Association (APA) (2021), caregivers are individuals, who provide unpaid care to a loved one who is in need of assistance due to a chronic illness, disability, or aging and are considered an essential part of the healthcare system (Schulz & Sherwood, 2008). These individuals often carry a significant burden, balancing their caregiving responsibilities with their own personal and professional obligations. As a result, family caregivers are at high risk for experiencing caregiver burnout, a state of physical, emotional, and mental exhaustion that can have severe consequences for both the caregiver and care recipient (APA, 2021; Caregiver Burnout, 2019). In addition to the significant emotional toll it takes on caregivers, burnout can have serious consequences for both caregivers and care recipients. For example, burnout can lead to a decline in the quality of care provided, which can negatively impact the health outcomes of the care recipient (Liu et al., 2020). Additionally, caregiver burnout has been linked to a range of negative health outcomes for the caregiver, including depression, anxiety, and physical illness (Schulz & Sherwood, 2008). Given the significant and potentially long-lasting effects of caregiver burnout, it is imperative that healthcare providers, policymakers, and researchers take steps to better understand this phenomenon and develop effective interventions to mitigate its impact. This article aims to provide an overview of caregiver burnout, its impact on caregivers and care recipients, and strategies for mitigating its effects.

Overview of Caregiver Burden and Burnout
Caregiver burden refers to the negative impact of caregiving on the caregiver's life, such as social isolation, financial strain, and disruptions to personal relationships (Liu et al., 2020). Both caregiver burden and burnout are prevalent issues that can have serious consequences for caregivers, care recipients, and the healthcare system as a whole. Caregiver burden can manifest in various ways, including financial strain, disruptions to personal relationships, social isolation, and decreased quality of life (Wilborn-Lee, 2015). Symptoms and effects of caregiver burnout and burden can vary depending on the individual caregiver, the care recipient's needs, and the duration and intensity of caregiving (Schulz & Eden, 2016). However, some common symptoms of caregiver burnout include emotional exhaustion, physical fatigue, depression, anxiety, and a decreased sense of personal accomplishment. (APA, 2021; “Caregiver Burnout, 2019; Smith, 2023). Factors that contribute to caregiver burnout and burden include the intensity and duration of caregiving, lack of support and resources, and the caregiver's own health status. Cleveland Clinic (2019) describe a variety of factors that contribute to caregiver burnout:
Role confusion: Many people are confused when thrust into the role of caregiver. It can be difficult for people to separate their role as caregivers from their roles as spouses, lovers, children, friends or other close relationships.
Unrealistic expectations: Many caregivers expect their involvement to have a positive effect on the health and happiness of the patient. This may be unrealistic for patients suffering from a progressive disease, such as Parkinson's or Alzheimer's.
Lack of control: Many caregivers become frustrated by a lack of money, resources and skills to effectively plan, manage and organize their loved one's care.
Unreasonable demands: Some caregivers place unreasonable burdens upon themselves, in part because they see providing care as their exclusive responsibility. Some family members such as siblings, adult children or the patient himself/herself may place unreasonable demands on the caregiver. They also may disregard their own responsibilities and place burdens on the person identified as primary caregiver.
Other factors: Many caregivers cannot recognize when they are suffering burnout and eventually get to the point where they cannot function effectively. They may even become sick themselves.
Caregiver burden can also negatively impact the care recipient, as the caregiver may experience difficulties in providing consistent and effective care. Additionally, caregiver burnout and burden can have an impact on the healthcare system as a whole, with implications for hospitalization rates, healthcare costs, and access to care (Ashley, 2017). Caregivers who provide care for extended periods, lack access to respite care, or have little support from family and friends may be at higher risk of experiencing caregiver burnout and burden. Caregivers who also have their own health concerns, such as chronic illness, may find it particularly challenging to provide care while maintaining their own health or may be at risk of neglecting their own health leading to long-term consequences (Reinhard et al., 2008). Additionally, the quality of care provided to the care recipient may decline as a result of caregiver burnout or burden, which can negatively impact the care recipient's health outcomes. From a healthcare system perspective, caregiver burnout and burden potentially lead to increased hospitalization rates and healthcare costs, as well as decreased access to care for the care recipient (Ashley, 2017).

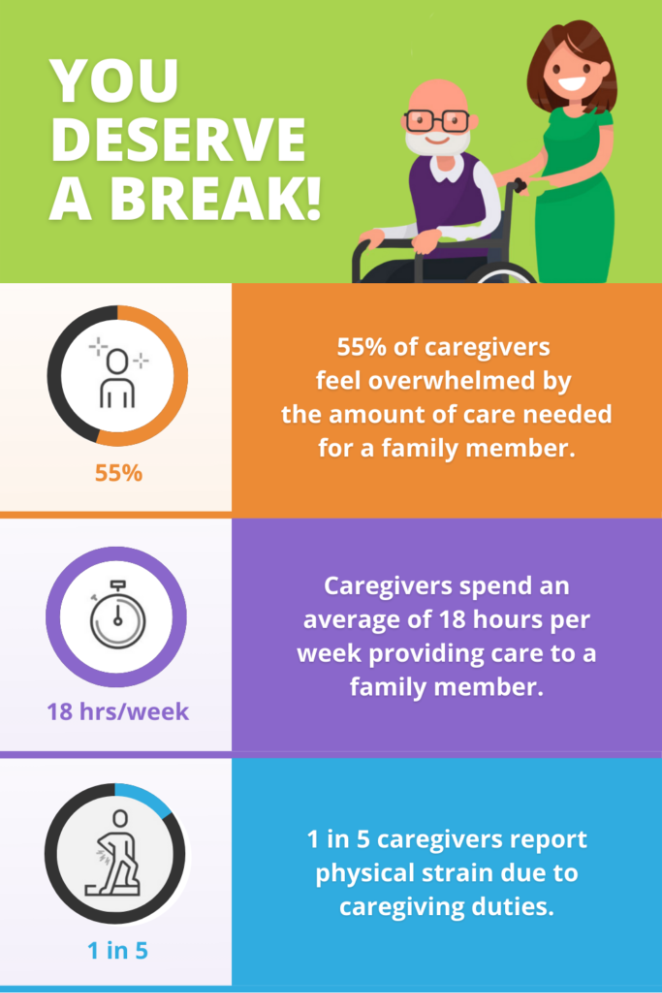
According to the AARP Public Policy Institute (2020), an estimated 48.9 million adults in the United States provided unpaid care to an adult family member or friend in 2020. The majority of these caregivers (59%) reported experiencing at least one burden associated with caregiving, such as financial strain, emotional stress, or time constraints. Additionally, about one in four caregivers reported high levels of emotional stress or strain, which can lead to caregiver burnout (AARP, 2020). Studies have shown that caregivers who experience high levels of stress or burnout are at increased risk of developing health problems themselves. For example, a study by Schulz and Beach (1999) found that caregivers who experience high levels of stress have a 63% higher mortality rate than non-caregivers of the same age. Caregivers also report higher rates of depression and anxiety than the general population (Pinquart & Sörensen, 2003). Caregiving can also have significant financial implications for caregivers. According to a report by the National Alliance for Caregiving and AARP (2015), caregivers in the United States spend an average of $7,000 per year on caregiving-related expenses, such as medications, transportation, and home modifications. Caregivers who work while providing care may also experience financial strain due to lost wages or reduced work hours (National Alliance for Caregiving & AARP, 2015).
In addition to the personal and financial impacts of caregiver burnout and burden, these issues also have implications for the healthcare system. Schulz and Beach (1999) also found that caregivers who experience high levels of stress are more likely to use healthcare services themselves, leading to higher healthcare costs. Additionally, caregiver burnout can lead to increased hospitalization rates for care recipients, which can further strain the healthcare system (National Alliance for Caregiving & AARP, 2015). Overall, these statistics highlight the significant impact of caregiver burnout and burden on caregivers, care recipients, and the healthcare system. It is important for policymakers, healthcare providers, and caregivers themselves to recognize the prevalence of these issues and work to identify effective strategies for mitigating their effects.
Ways to Mitigate Caregiver Burden and Burnout
There are several strategies that caregivers can use to mitigate burnout and manage stress. Research has found that interventions such as stress management programs and mindfulness training can be effective in reducing caregiver stress and improving well-being (Lloyd et al., 2020). Support systems such as respite care, counselling, and support groups can also provide much-needed relief for caregivers (AARP, 2021). Technological tools such as medication reminders, remote monitoring systems, and telehealth services can also assist caregivers in their role (Harris & Reid, 2020). Additionally, legislative policies such as the RAISE Family Caregivers Act, which was signed into law in 2018, aiming to support caregivers by providing resources and training to help them better navigate the caregiving journey (AARP, 2021). The RAISE Family Caregivers Act requires the development and implementation of a national strategy to support family caregivers. The act includes provisions for caregiver training, respite care, and other support services (AARP, 2021). By utilizing these strategies and resources, caregivers can better manage their responsibilities and reduce the risk of burnout and stress. In addition to the strategies mentioned, there are other interventions that have been found to be effective in mitigating caregiver burnout. For instance, psychoeducation and skills training interventions can help caregivers develop problem-solving and coping skills, and improve their ability to provide care (Wolff et al., 2016). Furthermore, caregiver support groups have been shown to be effective in reducing caregiver burden and improving mental health outcomes (Sörensen et al., 2011). Respite care, which provides caregivers with a temporary break from their caregiving responsibilities, has been identified as one of the most effective ways of preventing caregiver burnout (AARP, 2021). In addition to respite care, other support services such as counselling, therapy, and financial assistance can help alleviate caregiver burden and stress. Cleveland Clinic (2019) describe a variety of resources to mitigate caregiver burden and burnout:
Home health services: These agencies provide home health aides and nurses for short-term care, if your loved one is acutely ill. Some agencies provide short-term respite care.
Adult day care: These programs offer a place for seniors to socialize, engage in a variety of activities and receive needed medical care and other services.
Nursing homes or assisted living facilities: These institutions sometimes offer short-term respite stays to provide caregivers a break from their caregiving responsibilities.
Private care aides: These are professionals who specialize in assessing current needs and coordinating care and services.
Caregiver support services: These include support groups and other programs that can help caregivers recharge their batteries, meet others coping with similar issues, find more information, and locate additional resources.
Agency of Aging: The Agency of Aging is a government or non-profit organization that provides services and resources to older adults in a specific geographic area. The primary goal of these agencies is to support and enhance the well-being, independence, and quality of life of older adults. The specific services and programs offered by each Agency of Aging may vary depending on the needs and resources of the local community, but some common examples include caregiver support, transportation assistance, home-delivered meals, health promotion and disease prevention, legal assistance, and social activities.
National organizations: There are several national organizations in the United States that focus on caregiver burden and burnout. These organizations provide support, resources, and education to family caregivers to help them manage the challenges of caring for a loved one. One example is the Family Caregiver Alliance, a national organization that provides resources and support to family caregivers of adults with chronic or disabling conditions. They offer educational materials, online support groups, and a toll-free helpline staffed by trained professionals who can provide information and support.
Technology can also play a significant role in supporting caregivers. For example, mobile apps that offer medication reminders, care coordination tools, and symptom trackers can help caregivers better manage their care responsibilities (Harris & Reid, 2020). Telehealth services, which allow caregivers to connect with healthcare providers remotely, can also help reduce the burden of care and provide caregivers with additional support.

Further Research on Caregiver Burden and Burnout
Despite the growing recognition of caregiver burnout and burden, the research on this topic is still limited. Most of the current literature has focused on the prevalence and impact of caregiver burnout, as well as the factors that contribute to it. However, there is still much to be learned about effective interventions to mitigate caregiver burnout and burden. For example, while support groups have been found to be effective in reducing caregiver burden, more research is needed to identify the characteristics of successful support groups (Sörensen et al., 2011). Additionally, there is a need for more research on the long-term effects of caregiver burnout, as well as the impact of caregiver burnout on care recipients and the healthcare system as a whole (Reinhard et al., 2008). There are also several gaps in the literature on caregiver burnout. For instance, there is a lack of research on the experiences of minority caregivers, who may face unique challenges in providing care (National Alliance for Caregiving & AARP, 2020). Furthermore, there is a need for more research on the role of cultural and religious beliefs in shaping caregiver experiences and coping strategies (Gozalo et al., 2021). Future research directions should aim to address these gaps in the literature and identify effective interventions to support caregivers. This research could have important implications for policymakers, healthcare providers, and caregivers themselves. By identifying effective interventions and support systems, researchers can help reduce the burden of care and improve outcomes for both caregivers and care recipients.
Conclusion
In conclusion, caregiver burnout and burden are significant issues that can have wide-ranging effects on caregivers, care recipients, and the healthcare system. Identifying effective strategies for mitigating these effects is crucial for ensuring the well-being of both caregivers and care recipients, as well as the sustainability of the healthcare system. Various strategies for mitigating caregiver burnout include support systems, technological tools, and legislative policies. Despite the critical role of family caregivers and the potential risks associated with caregiver burnout, research on this topic is limited. The need for further research in this area includes identifying effective interventions long-term and addressing gaps in the literature. It is also crucial to understand these phenomena and identify effective strategies for mitigating the effects, which may include providing support and resources for caregivers and care recipients, as well as improving access to respite care and other services. From a healthcare system perspective, addressing caregiver burnout and burden may lead to better health outcomes for care recipients and reduced healthcare costs. (AARP Public Policy Institute, 2020; National Alliance for Caregiving & AARP, 2020.; Schulz & Sherwood, 2008; Wolff et al., 2016).
Bibliographical References
AARP Public Policy Institute. (2020). Caregiving in the United States 2020. https://www.aarp.org/ppi/info-2020/caregiving-in-the-united-states-2020.html
American Psychological Association. (2021). Caregivers. Retrieved from https://www.apa.org/pi/about/publications/caregivers/faq.
American Psychological Association. (2021). Caregiver burnout: Tips for taking care of yourself. Retrieved from https://www.apa.org/topics/caregiver-burnout
Ashley, C. (2017). Understanding Caregiver Burden and Hospital Use Among Older Home Care Recipients in Nova Scotia. Retrieved from https://dalspace.library.dal.ca/handle/10222/73534
Cleveland Clinic. (Reviewed 2019). Caregiver Burnout. Retrieved from https://my.clevelandclinic.org/health/diseases/9225-caregiver-burnout
Gozalo, P., Goldstein, N. E., Barreto, P., Keating, N. L., & McCarthy, E. P. (2021). Cultural and Religious Beliefs and Practices Among Family Caregivers of Older Adults: A Scoping Review. Journal of Applied Gerontology, 07334648211020218. Advance online publication. https://doi.org/10.1177/07334648211020218
Liu, Z., Heffernan, C., & Tan, J. (2020). Caregiver burden: A concept analysis. International journal of nursing sciences, 7(4), 438–445. https://doi.org/10.1016/j.ijnss.2020.07.012
National Alliance for Caregiving. (2020). Caregiving in the U.S. 2020. Retrieved from https://www.caregiving.org/caregiving-in-the-us-2020/
National Alliance for Caregiving & AARP. (2020). Caregiving in the U.S. https://www.aarp.org/content/dam/aarp/ppi/2020/05/full-report-caregiving-in-the-united-states.doi.10.26419-2Fppi.00103.001.pdf
National Alliance for Caregiving and AARP Public Policy Institute. (2015). Caregiving in the U.S. Retrieved from https://www.aarp.org/content/dam/aarp/ppi/2015/caregiving-in-the-united-states-2015-report-revised.pdf
Reinhard, S. C., Given, B., Petlick, N. H., & Bemis, A. (2008). Supporting Family Caregivers in Providing Care. In R. G. Hughes (Ed.), Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality (US).
Schulz, R., & Beach, S. R. (1999). Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA, 282(23), 2215-2219. https://doi.org/10.1001/jama.282.23.2215
Schulz, R., Eden, J., Committee on Family Caregiving for Older Adults, Board on Health Care Services, Health and Medicine Division, & National Academies of Sciences, Engineering, and Medicine (Eds.). (2016). Families Caring for an Aging America. National Academies Press (US).
Schulz, R., & Sherwood, P. R. (2008). Physical and mental health effects of family caregiving. American Journal of Nursing, 108(9 Suppl), 23-27. https://doi.org/10.1097/01.NAJ.0000336406.45248.4c
Smith, M. (Updated 2023). Caregiver Stress and Burnout. HelpGuide. Retrieved from https://www.helpguide.org/articles/stress/caregiver-stress-and-burnout.htm
Sörensen, S., Pinquart, M., & Duberstein, P. (2002). How effective are interventions with caregivers? An updated meta-analysis. Gerontologist, 42(3), 356-372. https://doi.org/10.1093/geront/42.3.356
Wilborn-Lee, B. (2015). The effects of stress and burden on caregivers of individuals with a chronic illness. Retrieved from https://scholarworks.waldenu.edu/cgi/viewcontent.cgi?article=2468&context=dissertations&httpsredir=1&referer=
Wolff, J. L., & Kasper, J. D. (2006). Caregivers of frail elders: Updating a national profile. The Gerontologist, 46(3), 344-356. https://doi.org/10.1093/geront/46.3.344
Visual Sources




Kommentarer