Loneliness: An Elusive Danger to Health
Loneliness is a complex and devastating emotional state described by a subjective sense of isolation or disconnection from meaningful social relationships. As social creatures, humans' inherent need for social interaction, support, and stimuli is integral to their well-being. However, the mere presence of these social elements does not guarantee a sense of belonging; instead, kinship is closely linked to the individual perception of one's social connections and interactions. This article delves into the complex repercussions of loneliness on various facets of health, from cardiovascular and metabolic consequences to immunologic responses. Loneliness leaves an indelible mark on mental health, too, with links to depression, dementia, suicidal thoughts, and personality disorders. As society moves to recognise loneliness as a public health concern, strategies and interventions become imperative (Cacioppo & Cacioppo, 2018).
Where Does It Come From?
Loneliness is caused when an individual's social network fails to align with their preferences, either in terms of quantity or attributes (Pop et al., 2022). The crux lies within this discrepancy between the objective reality of social presence and the subjective experience of belonging. While not classified as a clinical diagnosis, loneliness represents a significant psychological state that can affect both physiological and mental well-being, particularly when constant. This emotional state is not confined to specific life stages, yet heightened levels are often observed in late adolescence and among the elderly. An analogy can be made between loneliness and hunger, as the sensation of loneliness acts as a social parallel to the biological need for sustenance. Much like hunger triggers the imperative to eat, loneliness prompts an innate urge to establish new social relationships (Morr et al., 2022).
It is vital to recognise that loneliness is not synonymous with solitude. The size of one's social network does not necessarily shield against loneliness; an individual may feel isolated despite having an extensive and diverse social circle. Conversely, it is possible to lead a life with only a few meaningful social connections and experience no loneliness whatsoever. In a clinical setting, researchers examine what is known as "social isolation". This term typically refers to a state where a person experiences a reduction in both the quantity and quality of their interactions with others. This is an objective concept that can be assessed by observing an individual's social network (Benjamin & Gummanur, 2023; Freedman & Nicolle, 2020).
Impact on Health
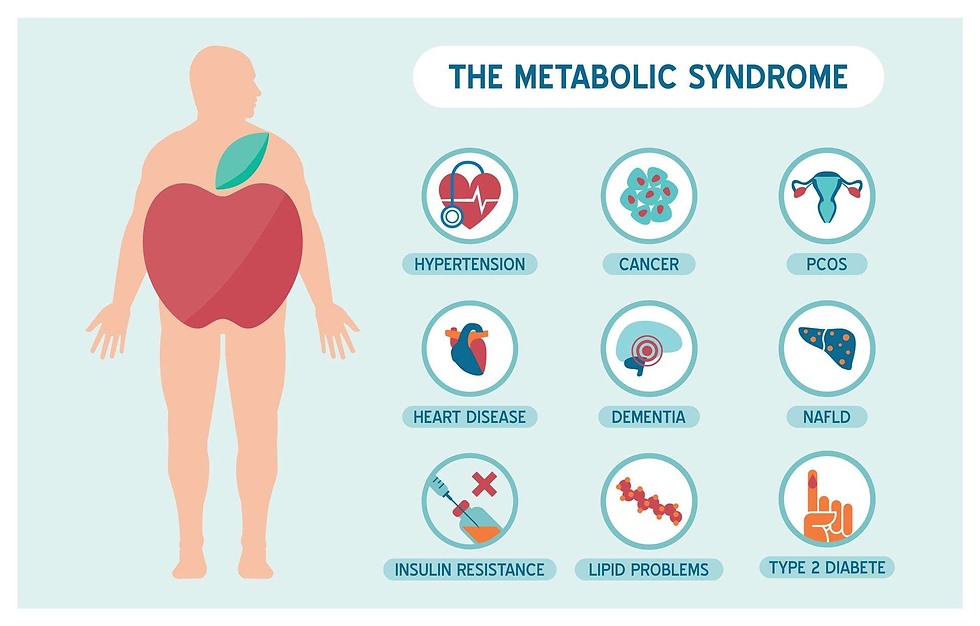
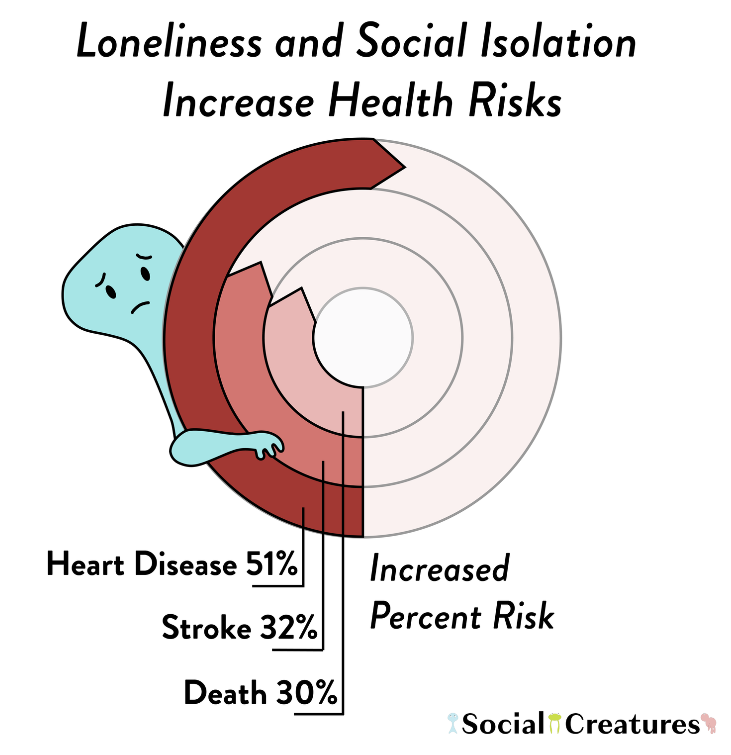
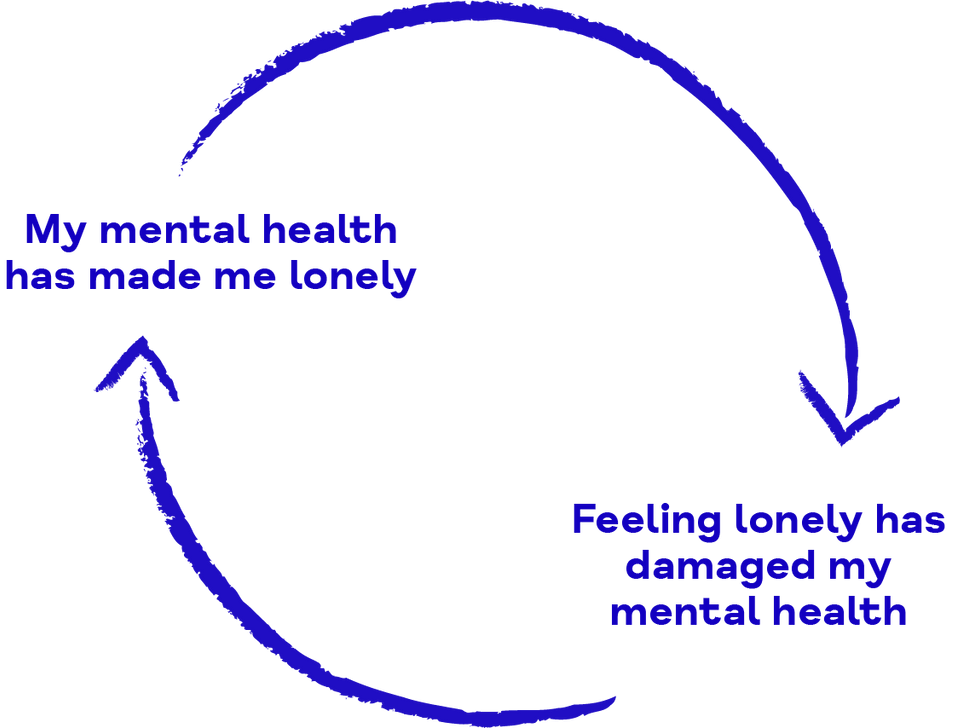
Long-lasting loneliness takes a toll on health. It is important to note that the adverse health effects linked to loneliness are not easily predicted just by looking at someone's level of social isolation or support. This fact sets loneliness apart from other concepts that are commonly mixed up with it (Cacioppo et al., 2010). Investigations reveal that loneliness can have severe effects on the cardiovascular system, contributing to conditions like coronary heart disease and stroke (Valtorta et al., 2016), while also exerting detrimental influences on brain health, potentially leading to dementia (Kuiper et al., 2015). Loneliness's link to metabolic syndrome (Whisman, 2010), often accompanied by depression (Henriksen et al., 2019), further underscores its systemic consequences. Alarmingly, loneliness has been correlated with increased mortality across various causes, increasing the likelihood of death by 26% in reported cases of loneliness (Holt-Lunstad et al., 2015). This evidence implies that loneliness operates systemically within the body, culminating in pathological consequences (Karelina & Devries, 2011).
It is currently believed that loneliness impacts health through three ‘pathways’: poor health behaviors, heightened stress response, and inadequate physiological repairing activity. The first one emphasises the fact that lonely individuals are more susceptible to developing unhealthy behaviours, such as smoking, decreased physical activity, and disrupted sleep patterns (Cacioppo et al., 2002; Hawkley et al., 2009).
Understanding stress and its impact on the body involves examining it from two angles: exposure and perception. The body interprets psychological stressors as threats and activates the sympathetic nervous system (SNS) and the hypothalamic-pituitary-adrenocortical (HPA) axis. Together, these systems set off an inflammatory response (Irwin & Cole, 2011). When perceived as a source of stress, loneliness becomes a catalyst for inflammatory processes, starting a physiological stress cascade. During acute stress situations, the initial activation of the SNS primes the immune system, mobilising leukocytes into the bloodstream. Simultaneously, stress-induced vagal withdrawal lowers acetylcholine levels, promoting inflammatory activity in tissues such as the liver, spleen, heart, and gastrointestinal tract. Acute psychological stressors release interleukin-1 beta (IL-1β), activating the HPA axis and releasing cortisol. Brain IL-1β, the leukocytic pyrogen, induces low-grade inflammation and elevated cytokine levels under severe stress. In moments of intense stress, the adrenal medulla releases epinephrine. This triggers the activation of corticotropin-releasing hormone, which, in turn, stimulates the sympathetic nervous system. This stimulation leads to an elevation in adrenocorticotropic hormone and the subsequent release of adrenocortical steroids (Pourriyahi et al., 2021).
Loneliness and Immunologic Factors
Although the stress response is a shared aspect of the human experience, its intensity varies among individuals (Hawkley & Cacioppo, 2003). Loneliness plays a significant role in shaping this reaction, as lonely individuals perceive routine events as more stressful than their non-lonely counterparts. This heightened perception is particularly evident in how social stressors contribute to increased levels of pro-inflammatory cytokines in the blood and the brain. As a result, those who are lonely exhibit a more pronounced increase, resulting in an elevated inflammatory response (Leschak & Eisenberger, 2019). Numerous studies have confirmed that individuals who experience loneliness exhibit a more pronounced increase in inflammation during stressful situations (Brown et al., 2018). This heightened response is associated with the conserved transcriptional response to adversity (Uchida et al., 2018), which not only can be triggered by loneliness but can also contribute to it, forming a reciprocal relationship between inflammation and perceived social stressors. The interplay between stress and challenging interpersonal relations appears to magnify inflammatory responses, particularly evident when faced with biologically demanding stressors such as endotoxin (Jaremka, Lindgren, et al., 2013).
Elevated interleukin-6 (IL-6) levels have also consistently been connected with loneliness (Balter et al., 2019; Smith et al., 2020). IL-6 is known for its diverse roles in promoting acute-phase reactants and regulating immune functions essential for acquired immunity. However, imbalanced production of IL-6 can have detrimental health effects and contribute to age-related diseases (Tanaka et al., 2014). Another pro-inflammatory cytokine, TNF-α, involved in immune response regulation and vascular processes, positively correlates with loneliness (Jaremka, Fagundes, et al., 2013). Loneliness is also associated with altered levels of interleukin-2 and interleukin-10, as seen in studies exploring the cytokine profile of breast cancer survivors and its connection to psychosomatic factors (Henneghan et al., 2020).
C-reactive protein (CRP) is a key marker for inflammation and infection and is extremely important in the immune response. It activates the complement system, recognises pathogens, and interacts with Fcγ receptors. Lonelier individuals have been shown to have higher CRP levels (Nersesian et al., 2018; Vingeliene et al., 2019). MCP-1 is a crucial chemokine that regulates monocyte and macrophage migration and is associated with inflammatory diseases. Those who experience loneliness, particularly women and those with type 2 diabetes, exhibit higher MCP-1 levels in response to mental stress, yet again showing higher inflammation rates as a consequence of loneliness (Hackett et al., 2019). In addition to inflammatory markers, loneliness also affects humoral immunity—elders experiencing loneliness exhibit reduced levels of immunoglobulins. Loneliness affects mucosal immunity, potentially making individuals more susceptible to infections, as evidenced by decreased salivary IgA levels linked to stress (Pourriyahi et al., 2021). Interferon levels are lower in lonely individuals, affecting antiviral defence—both type I and type II interferons are down-regulated in response to perceived social isolation. This suggests loneliness may compromise the body's ability to mount an effective immune response against viruses (Cole et al., 2015).
Loneliness and Metabolic and Cardiovascular Factors
Cortisol can be thought of as an indicator of psychological stress. This hormone follows a natural daily pattern, it peaks around 30 minutes after waking up and gradually decreases, reaching its lowest levels at midnight. This rhythmic pattern can be effectively measured using specific cortisol indices. The Cortisol Awakening Response (CAR) measures how much cortisol increases in the first 30 to 45 minutes after waking. The diurnal slope represents the rate at which cortisol decreases from its highest point in the morning to its lowest point. Loneliness has been correlated with alterations in cortisol dynamics, specifically showing an attenuated CAR (Lai et al., 2018).
Studies suggest an association between loneliness and type 2 diabetes mellitus (Foti et al., 2020), hyperglycaemia (Rico-Uribe et al., 2018), and elevated haemoglobin A1c (Shiovitz-Ezra & Parag, 2019) and fasting blood sugar levels (Whisman, 2010). Lonely individuals often have higher triglyceride levels (Abdellaoui et al., 2019) and lower high-density lipoprotein cholesterol (Badcock et al., 2019). Loneliness is also related to an increased body mass index and obesity (Keenan et al., 2018), including central obesity (Kwon et al., 2018), higher waist circumference, and greater body fat (Yen et al., 2018). Individuals with altered dietary habits due to loneliness exhibit increased food consumption and higher intake of sugary beverages (Henriksen et al., 2014), possibly tied to deregulated appetite-related hormones like ghrelin and leptin (Jaremka et al., 2018). Loneliness is further linked to hypertension (Rico-Uribe et al., 2018), which might cause elevated systolic (Kobos et al., 2020) and diastolic (Steptoe et al., 2004) blood pressures, altered cardiovascular function, and reduced autonomic cardiac control. These physiological manifestations contribute to higher rates of cardiovascular diseases, including coronary heart disease, stroke, and increased cardiovascular mortality (Stringhini et al., 2018). This holds true even for individuals with stable coronary heart disease receiving medication as secondary prevention (Hagström et al., 2018).
The Impact of Loneliness on Mental Health and Psychiatric Disorders
As aforementioned, loneliness, which is often overlooked, is more than just a feeling of being alone, as it has detrimental effects on mental well-being (West et al., 1986).
Loneliness and depression often intertwine, sharing common symptoms such as helplessness and emotional pain. Individuals experiencing loneliness are reported to suffer from more depressive symptoms, feeling less happy, satisfied, and more pessimistic. The overlap in the characteristics between these two reaches such a degree that some consider loneliness a subset of depression. However, a crucial distinction lies in the underlying hope of the lonely person – the belief that reunification with a longed-for person could remedy their situation. Nonetheless, depression and loneliness often appear in tandem (Mushtaq et al., 2014).
Loneliness emerges as a significant factor linked to an over two-fold increase in the risk of dementia, positioning itself as not only a consequence but potentially a prodromal stage of cognitive decline. The impact extends to a swifter deterioration in various cognitive areas, including global cognition, semantic memory, perceptual speed, and visuospatial ability (Holwerda et al., 2014). The association between loneliness and Alzheimer's disease can be explained in two ways. First, loneliness might be a consequence of dementia, perhaps as a response to diminished cognitive abilities or as a direct result of the pathology contributing to dementia. Second, loneliness could compromise the neural systems crucial for cognition and memory, making lonely individuals more vulnerable to the effects of age-related neuropathology and reducing neural reserves (Wilson et al., 2007).
Research on suicide has consistently shown a strong association between suicidal thoughts, self-harm, and loneliness. As the degree of loneliness increases, so does the prevalence of suicidal thoughts and self-harming behaviours. The peak season for loneliness corresponds to the peak season for suicide, which occurs in winter and spring. Notably, there are minimal gender differences concerning the link between loneliness and suicide (Stravynski & Boyer, 2001). Loneliness is also related to specific personality disorders, specifically borderline personality disorder (BPD) and schizoid personality disorder. In BPD, the intolerance of aloneness is a central feature that influences and amplifies other symptoms. Regarding schizoid personality disorder, the lack of emotional security and contentment in interpersonal relationships contributes to its manifestation (Mushtaq et al., 2014).
Loneliness: A Pandemic
Urbanisation, changes in communication patterns, and the development of social media have undoubtedly contributed to the reinforcement of loneliness. Despite being recognised as a public health concern and even being labelled as a pandemic, effectively addressing this issue remains incredibly difficult (Lonergan-Cullum et al., 2022; Pop et al., 2022).
Public awareness campaigns are a crucial strategy to educate communities about the detrimental effects of loneliness and advocate the cause of social inclusion. Loneliness remains a somewhat overlooked and stigmatised concept in the modern world; it is often viewed through a lens of negativity and embarrassment; therefore, opening up about it is challenging (Abdellaoui et al., 2019). Addressing loneliness at a societal level requires a shift in perspective and behaviour. The complexity and individuality of loneliness make it resistant to simple solutions. Rather than approaching it as a puzzle that needs to be solved, a more pragmatic stance involves efforts to make loneliness a less painful experience. This nuanced approach acknowledges the enduring nature of loneliness while fostering awareness and understanding to alleviate its impact (Vingeliene et al., 2019). Encouraging non-lonely individuals to extend small gestures—a smile or a kind word—to those who are perceived as lonely can make a significant difference. This way, one acknowledges, with compassion, the shared vulnerability of the human experience, recognising that everyone has been confronted with loneliness at some point (Killeen, 1998).
Strategies to Combat Loneliness
Experiencing periods of loneliness is an inherent part of the human journey, and it is crucial to recognise that these feelings do not imply inherent flaws. Life transitions (for example, graduating, moving, becoming a single parent, or being unemployed) can trigger a sense of isolation. Building self-esteem becomes pivotal in lessening the impact of loneliness, as low self-esteem can hinder social interactions. Engaging in manageable activities and progressively building upon them is a positive strategy. Staying occupied through volunteering or pursuing hobbies provides a sense of purpose and fosters connections with others, which eventually soothes loneliness. Exploring personal interests—participating in evening classes or sports—can be instrumental in redirecting focus from loneliness. Embracing solitude, although unfamiliar at first, can be a liberating experience, promoting self-reflection and confidence. It is essential to realise that feelings of loneliness are transient and may surface during different stages of life. Embracing these emotions and focusing on the present circumstances can be empowering. The internet should be used with caution. Online content can exacerbate feelings of inadequacy, as people often curate idealised versions of their lives. While online communities can be a way to socialise, spending time with people in person is also important. Relying on and trusting new online connections might be as beneficial as dangerous. Persistent and unexplained loneliness may signal underlying issues such as depression, necessitating open discussions with friends, family, counsellors, or healthcare professionals. There is nothing wrong with seeking professional help; trying to fix one's situation is a testament to resilience and the opposite of weakness (12 Ways to Beat Loneliness - Heart Matters Magazine - BHF, n.d.; Coping with Loneliness and Isolation - HSE.Ie, n.d.).
Conclusions
Loneliness is an underestimated and complex emotional state that has a profound impact on human well-being. Rooted in the misalignment between an individual's social preferences and reality, loneliness goes well beyond solitude. Its implications on health are alarming, with systemic consequences affecting cardiovascular, metabolic, and immunologic factors. Loneliness intensifies the stress response and compromises the immune system, leading to inflammation and susceptibility to infections. Mental health is especially susceptible. Depression, dementia, suicidal thoughts, and personality disorders are just the tip of the iceberg of potential consequences. The challenge lies in how we address loneliness as a societal issue to combat stigma and raise awareness. Public campaigns, a shift in perspective, and small gestures of kindness are crucial in mitigating loneliness. In an increasingly interconnected world where human connections often remain superficial, loneliness presents a substantial problem.
Bibliographical References
12 ways to beat loneliness - Heart Matters magazine - BHF. (n.d.). Retrieved December 16, 2023, from https://www.bhf.org.uk/informationsupport/heart-matters-magazine/wellbeing/dealing-with-loneliness
Abdellaoui, A., Sanchez-Roige, S., Sealock, J., Treur, J. L., Dennis, J., Fontanillas, P., Elson, S., Nivard, M. G., Ip, H. F., Van Der Zee, M., Baselmans, B. M. L., Hottenga, J. J., Willemsen, G., Mosing, M., Lu, Y., Pedersen, N. L., Denys, D., Amin, N., M Van Duijn, C., … Boomsma, D. I. (2019). Phenome-wide investigation of health outcomes associated with genetic predisposition to loneliness. Human Molecular Genetics, 28(22), 3853–3865. https://doi.org/10.1093/hmg/ddz219
Badcock, J. C., Mackinnon, A., Waterreus, A., Watts, G. F., Castle, D., McGrath, J. J., & Morgan, V. A. (2019). Loneliness in psychotic illness and its association with cardiometabolic disorders. Schizophrenia Research, 204, 90–95. https://doi.org/10.1016/j.schres.2018.09.021
Balter, L. J. T., Raymond, J. E., Aldred, S., Drayson, M. T., Veldhuijzen van Zanten, J. J. C. S., Higgs, S., & Bosch, J. A. (2019). Loneliness in healthy young adults predicts inflammatory responsiveness to a mild immune challenge in vivo. Brain, Behavior, and Immunity, 82, 298–301. https://doi.org/10.1016/j.bbi.2019.08.196
Benjamin, D. G., & Gummanur, P. (2023). Loneliness – Cancer of the Mind. In Indian Journal of Palliative Care (Vol. 29, Issue 2, pp. 212–216). Scientific Scholar. https://doi.org/10.25259/IJPC_200_2022
Brown, E. G., Gallagher, S., & Creaven, A. M. (2018). Loneliness and acute stress reactivity: A systematic review of psychophysiological studies. In Psychophysiology (Vol. 55, Issue 5, p. e13031). John Wiley & Sons, Ltd. https://doi.org/10.1111/psyp.13031
Cacioppo, J. T., & Cacioppo, S. (2018). The growing problem of loneliness. In The Lancet (Vol. 391, Issue 10119, p. 426). Lancet Publishing Group. https://doi.org/10.1016/S0140-6736(18)30142-9
Cacioppo, J. T., Hawkley, L. C., Berntson, G. G., Ernst, J. M., Gibbs, A. C., Stickgold, R., & Hobson, J. A. (2002). Do Lonely Days Invade the Nights? Potential Social Modulation of Sleep Efficiency. Psychological Science, 13(4), 384–387. https://doi.org/10.1111/1467-9280.00469
Cacioppo, J. T., Hawkley, L. C., & Thisted, R. A. (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the chicago health, aging, and social relations study. Psychology and Aging, 25(2), 453–463. https://doi.org/10.1037/a0017216
Cole, S. W., Capitanio, J. P., Chun, K., Arevalo, J. M. G., Ma, J., & Cacioppo, J. T. (2015). Myeloid differentiation architecture of leukocyte transcriptome dynamics in perceived social isolation. Proceedings of the National Academy of Sciences of the United States of America, 112(49), 15142–15147. https://doi.org/10.1073/pnas.1514249112
Coping with loneliness and isolation - HSE.ie. (n.d.). Retrieved December 16, 2023, from https://www2.hse.ie/mental-health/life-situations-events/loneliness/coping-with/
Foti, S. A., Khambaty, T., Birnbaum-Weitzman, O., Arguelles, W., Penedo, F., Espinoza Giacinto, R. A., Gutierrez, A. P., Gallo, L. C., Giachello, A. L., Schneiderman, N., & Llabre, M. M. (2020). Loneliness, Cardiovascular Disease, and Diabetes Prevalence in the Hispanic Community Health Study/Study of Latinos Sociocultural Ancillary Study. Journal of Immigrant and Minority Health, 22(2), 345–352. https://doi.org/10.1007/s10903-019-00885-7
Freedman, A., & Nicolle, J. (2020). Social isolation and loneliness: The new geriatric giants Approach for primary care. In Canadian Family Physician (Vol. 66, Issue 3, pp. 176–182). College of Family Physicians of Canada. /pmc/articles/PMC8302356/
Hackett, R. A., Poole, L., Hunt, E., Panagi, L., & Steptoe, A. (2019). Loneliness and biological responses to acute stress in people with Type 2 diabetes. Psychophysiology, 56(6), e13341. https://doi.org/10.1111/psyp.13341
Hagström, E., Norlund, F., Stebbins, A., Armstrong, P. W., Chiswell, K., Granger, C. B., López-Sendón, J., Pella, D., Soffer, J., Sy, R., Wallentin, L., White, H. D., Stewart, R. A. H., & Held, C. (2018). Psychosocial stress and major cardiovascular events in patients with stable coronary heart disease. Journal of Internal Medicine, 283(1), 83–92. https://doi.org/10.1111/joim.12692
Hawkley, L. C., & Cacioppo, J. T. (2003). Loneliness and pathways to disease. Brain, Behavior, and Immunity, 17(1 SUPPL.), 98–105. https://doi.org/10.1016/S0889-1591(02)00073-9
Hawkley, L. C., Thisted, R. A., & Cacioppo, J. T. (2009). Loneliness Predicts Reduced Physical Activity: Cross-Sectional & Longitudinal Analyses. Health Psychology, 28(3), 354–363. https://doi.org/10.1037/a0014400
Henneghan, A., Haley, A. P., & Kesler, S. (2020). Exploring Relationships Among Peripheral Amyloid Beta, Tau, Cytokines, Cognitive Function, and Psychosomatic Symptoms in Breast Cancer Survivors. Biological Research for Nursing, 22(1), 126–138. https://doi.org/10.1177/1099800419887230
Henriksen, R. E., Nilsen, R. M., & Strandberg, R. B. (2019). Loneliness as a risk factor for metabolic syndrome: Results from the HUNT study. Journal of Epidemiology and Community Health, 73(10), 941–946. https://doi.org/10.1136/jech-2019-212335
Henriksen, R. E., Torsheim, T., & Thuen, F. (2014). Loneliness, social integration and consumption of sugar-containing beverages: Testing the social baseline theory. PLoS ONE, 9(8), e104421. https://doi.org/10.1371/journal.pone.0104421
Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., & Stephenson, D. (2015). Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspectives on Psychological Science, 10(2), 227–237. https://doi.org/10.1177/1745691614568352
Holwerda, T. J., Deeg, D. J. H., Beekman, A. T. F., Van Tilburg, T. G., Stek, M. L., Jonker, C., & Schoevers, R. A. (2014). Feelings of loneliness, but not social isolation, predict dementia onset: Results from the Amsterdam Study of the Elderly (AMSTEL). Journal of Neurology, Neurosurgery and Psychiatry, 85(2), 135–142. https://doi.org/10.1136/jnnp-2012-302755
Irwin, M. R., & Cole, S. W. (2011). Reciprocal regulation of the neural and innate immune systems. In Nature Reviews Immunology (Vol. 11, Issue 9, pp. 625–632). Nature Publishing Group. https://doi.org/10.1038/nri3042
Jaremka, L. M., Fagundes, C. P., Peng, J., Bennett, J. M., Glaser, R., Malarkey, W. B., & Kiecolt-Glaser, J. K. (2013). Loneliness Promotes Inflammation During Acute Stress. Psychological Science, 24(7), 1089–1097. https://doi.org/10.1177/0956797612464059
Jaremka, L. M., Lebed, O., & Sunami, N. (2018). Threats to Belonging, Immune Function, and Eating Behavior: an Examination of Sex and Gender Differences. In Current Psychiatry Reports (Vol. 20, Issue 9, pp. 1–7). Current Medicine Group LLC 1. https://doi.org/10.1007/s11920-018-0939-2
Jaremka, L. M., Lindgren, M. E., & Kiecolt-Glaser, J. K. (2013). Synergistic relationships among stress, depression, and troubled relationships: Insights from psychoneuroimmunology. Depression and Anxiety, 30(4), 288–296. https://doi.org/10.1002/da.22078
Karelina, K., & Devries, A. C. (2011). Modeling social influences on human health. Psychosomatic Medicine, 73(1), 67–74. https://doi.org/10.1097/PSY.0B013E3182002116
Keenan, K., Wroblewski, K., Matthews, P. A., Hipwell, A. E., & Stepp, S. D. (2018). Differences in childhood body mass index between lesbian/gay and bisexual and heterosexual female adolescents: A follow-back study. PLoS ONE, 13(6), e0196327. https://doi.org/10.1371/journal.pone.0196327
Killeen, C. (1998). Loneliness: An epidemic in modern society. Journal of Advanced Nursing, 28(4), 762–770. https://doi.org/10.1046/j.1365-2648.1998.00703.x
Kobos, E., Szewczyk, A., Świątkowska, T., Kryczka, T., & Sienkiewicz, Z. (2020). Relationship between loneliness and blood glucose control in diabetes. BMC Public Health, 20(1), 1–6. https://doi.org/10.1186/s12889-020-09241-z
Kuiper, J. S., Zuidersma, M., Oude Voshaar, R. C., Zuidema, S. U., van den Heuvel, E. R., Stolk, R. P., & Smidt, N. (2015). Social relationships and risk of dementia: A systematic review and meta-analysis of longitudinal cohort studies. In Ageing Research Reviews (Vol. 22, pp. 39–57). Elsevier. https://doi.org/10.1016/j.arr.2015.04.006
Kwon, A. R., Yoon, Y. S., Min, K. P., Lee, Y. K., & Jeon, J. H. (2018). Eating alone and metabolic syndrome: A population-based Korean National Health and Nutrition Examination Survey 2013–2014. Obesity Research and Clinical Practice, 12(2), 146–157. https://doi.org/10.1016/j.orcp.2017.09.002
Lai, J. C. L., Leung, M. O. Y., Lee, D. Y. H., Lam, Y. W., & Berning, K. (2018). Loneliness and diurnal salivary cortisol in emerging adults. International Journal of Molecular Sciences, 19(7), 1944. https://doi.org/10.3390/ijms19071944
Leschak, C. J., & Eisenberger, N. I. (2019). Two Distinct Immune Pathways Linking Social Relationships With Health: Inflammatory and Antiviral Processes. Psychosomatic Medicine, 81(8), 711–719. https://doi.org/10.1097/PSY.0000000000000685
Lonergan-Cullum, M., Hooker, S. A., Levy, R., & Ricco, J. (2022). A New Pandemic of Loneliness. Journal of the American Board of Family Medicine, 35(3), 593–596. https://doi.org/10.3122/jabfm.2022.03.210461
Morr, M., Liu, X., Hurlemann, R., Becker, B., & Scheele, D. (2022). Chronic Loneliness: Neurocognitive Mechanisms and Interventions. In Psychotherapy and Psychosomatics (Vol. 91, Issue 4, pp. 227–237). S. Karger AG. https://doi.org/10.1159/000524157
Mushtaq, R., Shoib, S., Shah, T., & Mushtaq, S. (2014). Relationship between loneliness, Psychiatric disorders and physical health ? A review on the psychological aspects of loneliness. In Journal of Clinical and Diagnostic Research (Vol. 8, Issue 9, pp. WE01–WE04). JCDR Research & Publications Private Limited. https://doi.org/10.7860/JCDR/2014/10077.4828
Nersesian, P. V., Han, H. R., Yenokyan, G., Blumenthal, R. S., Nolan, M. T., Hladek, M. D., & Szanton, S. L. (2018). Loneliness in middle age and biomarkers of systemic inflammation: Findings from Midlife in the United States. Social Science and Medicine, 209, 174–181. https://doi.org/10.1016/j.socscimed.2018.04.007
Pop, L. M., Iorga, M., & Iurcov, R. (2022). Body-Esteem, Self-Esteem and Loneliness among Social Media Young Users. International Journal of Environmental Research and Public Health, 19(9). https://doi.org/10.3390/ijerph19095064
Pourriyahi, H., Yazdanpanah, N., Saghazadeh, A., & Rezaei, N. (2021). Loneliness: An immunometabolic syndrome. In International Journal of Environmental Research and Public Health (Vol. 18, Issue 22). Multidisciplinary Digital Publishing Institute (MDPI). https://doi.org/10.3390/ijerph182212162
Rico-Uribe, L. A., Caballero, F. F., Martín-María, N., Cabello, M., Ayuso-Mateos, J. L., & Miret, M. (2018). Association of loneliness with all-cause mortality: A meta-analysis. PLOS ONE, 13(1), e0190033. https://doi.org/10.1371/JOURNAL.PONE.0190033
Shiovitz-Ezra, S., & Parag, O. (2019). Does loneliness ‘get under the skin’? Associations of loneliness with subsequent change in inflammatory and metabolic markers. Aging and Mental Health, 23(10), 1358–1366. https://doi.org/10.1080/13607863.2018.1488942
Smith, K. J., Gavey, S., RIddell, N. E., Kontari, P., & Victor, C. (2020). The association between loneliness, social isolation and inflammation: A systematic review and meta-analysis. In Neuroscience and Biobehavioral Reviews (Vol. 112, pp. 519–541). Pergamon. https://doi.org/10.1016/j.neubiorev.2020.02.002
Steptoe, A., Owen, N., Kunz-Ebrecht, S. R., & Brydon, L. (2004). Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology, 29(5), 593–611. https://doi.org/10.1016/S0306-4530(03)00086-6
Stravynski, A., & Boyer, R. (2001). Loneliness in Relation to Suicide Ideation and Parasuicide: A Population‐Wide Study. Suicide and Life-Threatening Behavior, 31(1), 32–40. https://doi.org/10.1521/suli.31.1.32.21312
Stringhini, S., Zaninotto, P., Kumari, M., Kivimäki, M., Lassale, C., & Batty, G. D. (2018). Socio-economic trajectories and cardiovascular disease mortality in older people: The English Longitudinal Study of Ageing. International Journal of Epidemiology, 47(1), 36–46. https://doi.org/10.1093/ije/dyx106
Tanaka, T., Narazaki, M., & Kishimoto, T. (2014). Il-6 in inflammation, Immunity, And disease. Cold Spring Harbor Perspectives in Biology, 6(10), a016295. https://doi.org/10.1101/cshperspect.a016295
Uchida, Y., Kitayama, S., Akutsu, S., Park, J., & Cole, S. W. (2018). Optimism and the conserved transcriptional response to adversity. Health Psychology, 37(11), 1077–1080. https://doi.org/10.1037/hea0000675
Valtorta, N. K., Kanaan, M., Gilbody, S., Ronzi, S., & Hanratty, B. (2016). Loneliness and social isolation as risk factors for coronary heart disease and stroke: Systematic review and meta-analysis of longitudinal observational studies. In Heart (Vol. 102, Issue 13, pp. 1009–1016). BMJ Publishing Group Ltd and British Cardiovascular Society. https://doi.org/10.1136/heartjnl-2015-308790
Vingeliene, S., Hiyoshi, A., Lentjes, M., Fall, K., & Montgomery, S. (2019). Longitudinal analysis of loneliness and inflammation at older ages: English longitudinal study of ageing. Psychoneuroendocrinology, 110, 104421. https://doi.org/10.1016/j.psyneuen.2019.104421
West, D. A., Kellner, R., & Moore-West, M. (1986). The effects of loneliness: A review of the literature. In Comprehensive Psychiatry (Vol. 27, Issue 4, pp. 351–363). Compr Psychiatry. https://doi.org/10.1016/0010-440X(86)90011-8
Whisman, M. A. (2010). Loneliness and the Metabolic Syndrome in a Population-Based Sample of Middle-Aged and Older Adults. Health Psychology, 29(5), 550–554. https://doi.org/10.1037/a0020760
Wilson, R. S., Krueger, K. R., Arnold, S. E., Schneider, J. A., Kelly, J. F., Barnes, L. L., Tang, Y., & Bennett, D. A. (2007). Loneliness and risk of Alzheimer disease. Archives of General Psychiatry, 64(2), 234–240. https://doi.org/10.1001/archpsyc.64.2.234
Yen, Y., Shi, Y., Soeung, B., Seng, R., Dy, C., Suy, R., & Ngin, K. (2018). The associated risk factors for underweight and overweight high school students in Cambodia. Diabetes and Metabolic Syndrome: Clinical Research and Reviews, 12(5), 737–742. https://doi.org/10.1016/j.dsx.2018.04.016









Loneliness can profoundly impact mental and physical health, highlighting the importance of social connections and emotional support in maintaining well-being. Understanding the complexities of loneliness underscores its effects on health outcomes, emphasizing the need for strategies and interventions to foster meaningful social interactions. It provides valuable insights into mental health and well-being, complemented by information on natural remedies like Essiac Tea dosage which can support overall health and emotional resilience.