The Urgency of a Stroke
- Holly Bennett
- Jan 8, 2023
- 6 min read
Updated: Feb 26, 2023
A cerebrovascular accident (CVA), or stroke, is a neurological disorder that is caused when a blood vessel is either blocked by a blood clot or ruptures ("About stroke," n.d.). This disruption in blood flow leads to a lack of oxygen traveling to the brain and results in brain cell death. An obstruction of blood flow by a clot is referred to as an ischemic stroke, and when a blood vessel ruptures it is diagnosed as a hemorrhagic stroke. Strokes have been linked with dementia and depression, as the disorder can leave many with severe impairments. (Kuriakose & Xiao, 2020). Blood flow to the brain consists of two internal carotid arteries and two vertebral arteries (Purves et al., 2001). These arteries go on to form the Circle of Willis. Neurons, or ‘brain cells’, are very sensitive to decreases in oxygen supply. Compromised blood flow to the brain can cause cell change quickly and lead to cell death and degeneration if the lack of blood supply is sustained. Prolonged periods of deprived oxygen and blood supply result in physical and cognitive impairment such as paralysis, language deficit, and movement disorder ("Effects of a stroke," n.d.).
Stroke is the second leading cause of death globally affecting approximately 13.7 million individuals per year. (Kuriakose & Xiao, 2020). The incidence of stroke is around 18.6% in people aged 20-54 years, and it doubles with age after 55 years. The prevalence of stroke in men versus women is also dependent on age, as incidence is higher at younger ages in women and slightly higher with older age in men. Women experience a higher risk for stroke due to factors associated with pregnancy, use of contraceptives, and hormonal therapy. Common causes of stroke in men include tobacco smoking, excessive alcohol use, myocardial infarctions, and arterial disease ("Stroke facts," 2022). Socioeconomic status has also been shown to have an inverse relationship with strokes. Low-income populations experience a higher incidence of stroke due to inadequate access to healthcare and a lack of post-stroke care (Nguyen-Huynh & Ovbiagle, 2011).

In addition, there are many risk factors contributing to stroke that are both non-modifiable and modifiable. Non-modifiable factors are factors that an individual is unable to control or adjust such as sex, age, and genetics. Modifiable factors are able to be managed or adjusted like smoking, diet, and physical inactivity. Smoking, in particular, is a significant modifiable risk factor for stroke as it is heavily linked to vascular injury and cerebrovascular disease. Studies have shown that smoking cessation significantly decreases vascular injury risk within a few months of cessation (Caprio & Sorond, 2019). Physical inactivity and poor diet are also well-known risk factors for stroke. Lifestyle adjustments such as increasing exercise and diet modifications have shown a 55% decrease in the risk of stroke (Kuriakose and Xiao, 2020).
Hypertension is another notable modifiable risk factor for stroke as excessive pressure and force on the arterial walls can cause tears ("High blood pressure," n.d.). The body then attempts to heal the tears with scar tissue which has been shown to capture foreign materials and produce plaque. This build-up begins to create blockages in arteries, which can lead to a stroke. Factors that cause hypertension include age, family history, sedentary lifestyle, and poor diet. Moreover, diabetes is also an impactful modifiable risk factor as people with diabetes are at double the risk of an ischemic stroke (Kuriakose & Xiao, 2020). Prognosis has been demonstrated to be worse in diabetics versus non-diabetics, with the former suffering higher chances of delayed recovery and severe impairment. The hormone, insulin, allows cells to absorb glucose that is present in the bloodstream for energy ("Pancreas hormones," 2022). A lack of insulin produced in diabetic patients causes an excess of glucose in the bloodstream which can increase clots in blood vessels ("Diabetes and stroke prevention," n.d.).

Strokes can be categorized as hemorrhagic and ischemic. A hemorrhagic stroke occurs when there is a rupture of a blood vessel, causing bleeding in the brain. Progression and expansion of a hemorrhagic stroke are correlated with severe damage to neurological function (Unnithan et al., 2022). Hemorrhagic strokes are generally caused by a weak vessel that tears and bleeds in the surrounding area of the brain ("Hemorrhagic stroke," n.d.). This leakage causes an accumulation and pressure on surrounding brain tissue. Arteriovenous malformations (AVMs) are also a significant cause of hemorrhagic stroke. AVMs are considered a tangled cluster of malformed blood vessels in the brain. These vessels have a higher chance of rupture, thereby resulting in a hemorrhagic stroke.
Ischemic strokes are estimated to occur in approximately 85% of stroke cases (Kuriakose & Xiao, 2020). It is caused by either thrombosis or an embolism which creates a blockage within a blood vessel in the brain. In thrombosis, blood clots are formed at the vessel walls, narrowing the amount of blood flow due to clot buildup (Ashorobi et al., 2022). Atherosclerosis, the process of fatty deposits accumulating on arterial walls, causes blood clots to form from the fatty plaque ("Ischemic stroke," n.d.). The thickening of the arterial walls of fatty deposits narrows the vessels, decreasing the amount of blood received by the brain. On the other hand, a stroke is caused by an embolism when a blood clot that has broken off a vessel wall or foreign material gets dislodged within a blood vessel, decreasing blood flow and oxygen to the brain. A blood clot is usually formed at another location in the body, commonly in the heart and large arteries located in the neck and upper chest area ("Ischemic stroke," n.d.). The clot then travels through the vessels of the brain until the vessels become too small for the clot to pass, restricting blood flow in that area.

Diagnostic testing for stroke consists of imaging and blood flow tests ("Let's talk about hemorrhagic stroke," 2022). Imaging includes computed tomography (CT) and magnetic resonance imaging (MRI) which help healthcare providers locate the extent of injury caused by the stroke. Blood flow tests such as cerebral angiography are able to provide information on the condition of one’s blood vessels and assist in finding the size and location of a vessel blockage. Diagnosis of a stroke is crucial when one experiences an acute stroke as patient prognosis is dependent on the time of treatment from symptom onset.
One of the most common treatments for an ischemic stroke is the use of alteplase (r-tPA), a drug that works to dissolve the blood clot disrupting blood flow. However, it is important to note that a healthcare provider must diagnose an individual with an ischemic stroke within 3 to 4.5 hours of symptom onset for the drug to be effective ("Let's talk about stroke," 2020). Mechanical thrombectomy is another choice of treatment used for blood clots that are larger in size. This procedure needs to be completed within 24 hours of symptom onset. Furthermore, treatment for a hemorrhagic stroke requires immediate care as surgery may be warranted dependent on the cause. Surgical intervention includes clipping the vessel at the base of the burst or removing abnormal blood vessels that are causing hemorrhage ("Let's talk about hemorrhagic stroke," 2022). If a stroke is caused by a blood clot, a wire-cage device referred to as a stent retriever is threaded into an artery to retrieve the clot and remove it from the circulatory system. Furthermore, there has been research investigating gene and stem cell therapy as treatment options for stroke. Studies have shown that gene therapy can improve the effects of an ischemic stroke by inhibiting proteins involved in cell death. Stem cell therapy has been shown to be effective in subacute or chronic stages of stroke. The therapy is able to target neural plasticity, inflammation, and promote new vascularization (Matei et al., 2021).
A stroke is regarded as a medical emergency and should be treated immediately when an individual begins to experience symptoms of a stroke. The American Stroke Association (2020) defined the warnings signs of stroke as:
Sudden numbness or weakness of the face, arm, or leg, especially on one side of the body
Sudden confusion, trouble speaking or understanding
Sudden trouble seeing in one or both eyes
Sudden trouble walking, dizziness, loss of balance or coordination
Sudden severe headache with no known cause
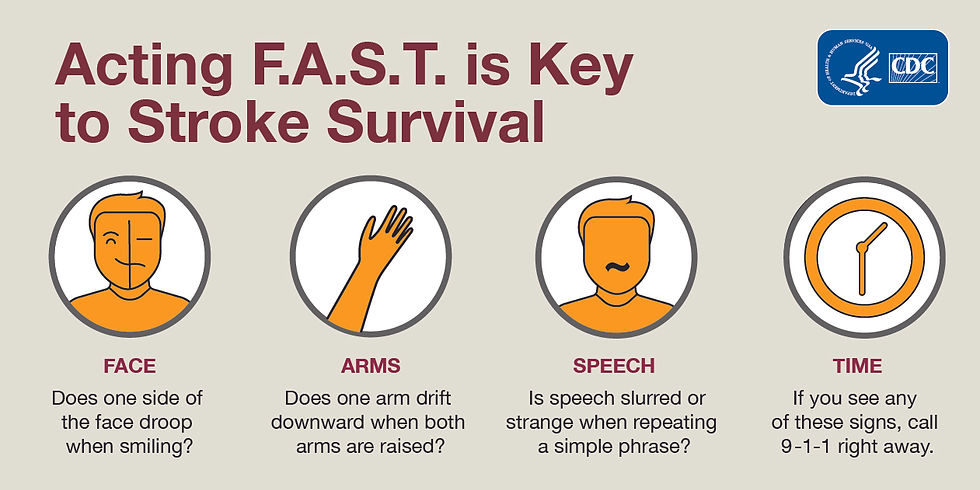
The association uses the acronym F.A.S.T for individuals to recognize signs of stroke: Face drooping, arm numbness, speech difficulty, and time to call 911.
All in all, stroke is considered a neurological disease where there is blockage or disruption in blood vessels that lead to the brain ("About stroke," n.d.). A lack of blood flow causes deprivation of oxygen and nutrients to brain cells, eventually leading to cell death and degeneration. It is vital to recognize the warning signs of a stroke for urgent medical treatment to prevent downstream neurological damage. Imaging and blood flow tests assist clinicians in diagnosing the type of stroke as well as deciding the appropriate treatment options.
Bibliographical References
About stroke. (n.d.). American Stroke Association. https://www.stroke.org/en/about-stroke
Ashorobi, D., Ameer , M. A., & Fernandez, R. (2022). Thrombosis. In StatPearls. StatPearls Publishing
Caprio, F. Z., & Sorond, F. A. (2019). Cerebrovascular disease: primary and secondary stroke prevention. The Medical Clinics of North America, 103(2), 295–308. https://doi.org/10.1016/j.mcna.2018.10.001
Diabetes and stroke prevention. (n.d.). American Stroke Association. https://www.stroke.org/en/about-stroke/stroke-risk-factors/diabetes-and-stroke-prevention
Effects of a stroke. (n.d.). John Hopkins Medicine. https://www.hopkinsmedicine.org/health/conditions-and-diseases/stroke/effects-of-stroke
Hemorrhagic strokes (bleeds). (n.d.). American Stroke Association. https://www.stroke.org/en/about-stroke/types-of-stroke/hemorrhagic-strokes-bleeds
High blood pressure and stroke. (n.d.). American Stroke Association. https://www.stroke.org/en/about-stroke/stroke-risk-factors/high-blood-pressure-and-stroke
Ischemic stroke (clots). (n.d.). American Stroke Association. https://www.stroke.org/en/about-stroke/types-of-stroke/ischemic-stroke-clots
Kuriakose, D., & Xiao, Z. (2020). Pathophysiology and treatment of stroke: present status and future perspectives. International Journal of Molecular Sciences, 21(20), 7609. https://doi.org/10.3390/ijms21207609
Let’s talk about hemorrhagic stroke. (2022). American Stroke Association. https://www.stroke.org/-/media/Stroke-Files/Lets-Talk-About-Stroke/Type-of-Stroke/LTAS-Hemorrhagic-Stroke.pdf
Let’s talk about stroke, TIA and warning signs. (2020). American Stroke Association. https://www.stroke.org/-/media/Stroke-Files/Lets-Talk-About-Stroke/About-Stroke/Lets-Talk-about-Stroke-TIA-Warning-Signs.pdf
Matei, N., Camara, J., & Zhang, J. H. (2021). The next step in the treatment of stroke. Frontiers in Neurology, 11, 582605. https://doi.org/10.3389/fneur.2020.582605
Ovbiagele, B., & Nguyen-Huynh, M. N. (2011). Stroke epidemiology: advancing our understanding of disease mechanism and therapy. Neurotherapeutics : The Journal of the American Society for Experimental NeuroTherapeutics, 8(3), 319–329. https://doi.org/10.1007/s13311-011-0053-1
Pancreas hormones. (2022, January 24). Endocrine Society. https://www.endocrine.org/patient-engagement/endocrine-library/hormones-and-endocrine-function/pancreas-hormones
Purves D, Augustine GJ, Fitzpatrick D, et al. (2001). The Blood Supply of the Brain and Spinal (2nd ed). Sinauer Associates. https://www.ncbi.nlm.nih.gov/books/NBK11042/
Stroke facts. (2022, October 14). Center of Disease Control and Prevention. https://www.cdc.gov/stroke/facts.htm
Unnithan, AKA., M Das, J., & Mehta, P. (2022). Hemorrhagic stroke. In StatPearls. StatPearls Publishing.
Visual Sources




Comments